Researchers at the University of Cincinnati College of Medicine have shown that a topical drug, called AB569, kills antibiotic-resistant bacteria and enhances would healing in burn injuries, according to Medical Xpress.
AB569, a combination of acidified nitrite and EDTA (ethylenediaminetetraacetic acid), was patented in the United States in 2018 by Dr. Daniel Hassett of the UC College of Medicine.
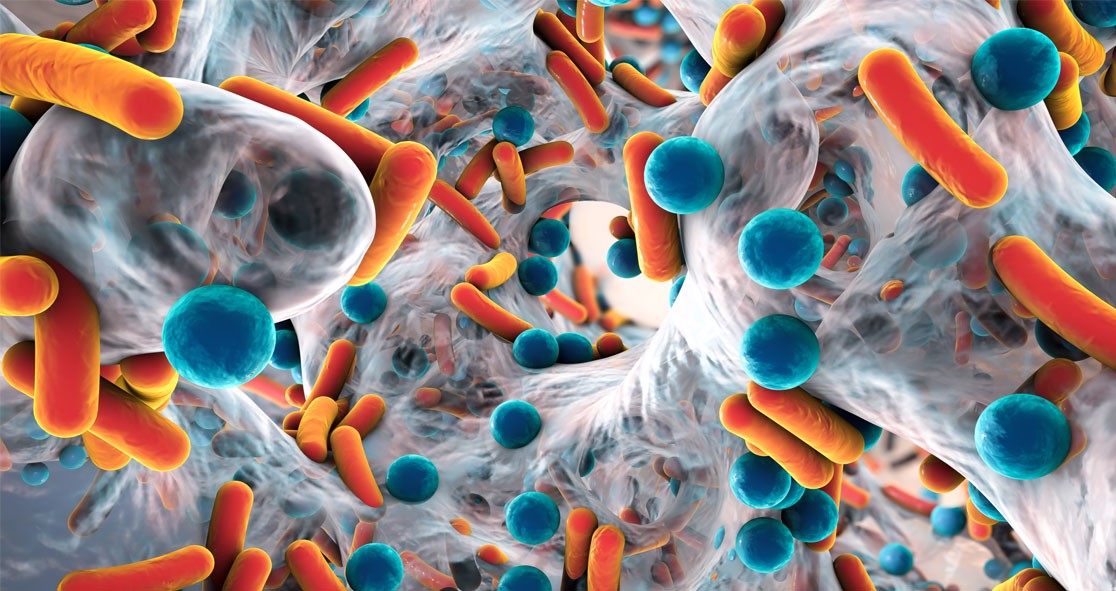
Dr. Hassett’s research has found that the topical drug kills virtually all pathogenic bacteria, including multidrug-resistant Pseudomonas aeruginosa (MDR-PA).
“Multidrug-resistant bacteria, often called ‘superbugs,’ are an ever-burgeoning global health problem,” Dr. Hassett said. “As a result, there is a critical need to develop novel and effective antimicrobials for the prevention, treatment and eradication and healing of such wounds that are complicated by the most formidable pathogen of burn patients, known as MDR-PA.”
“Injury severity is predominantly due to potentially lethal sepsis caused by MDR-PA,” he added.
The study, published in the journal Infection and Immunity, explained that AB569 acts synergistically to kill all human burn wound strains of the pathogen in vitro.
Dr. Hassett said, “AB569 not only kills the bug, it also enhances the wound-healing process. At the same time, AB569 topical application significantly increases the anti-inflammatory mediators … that allow improved epidermal restoration and the healing process to occur more rapidly and efficiently.”
Initially, the topical drug was seen as a potential treatment for antibiotic-resistant organisms that cause pulmonary infections in patients with cystic fibrosis and chronic obstructive pulmonary disease (COPD).
Apart from tackling cystic fibrosis and COPD, AB569 may also be effective in treating infections related to severe burns, urinary tract disorders, endocarditis, and diabetes, according to Dr. Hassett.
He said, “This study provides solid foundational evidence that AB569 can be used topically to treat highly problematic dermal [injuries] including wound, burn, blast and likely diabetic infections in civilian and military populations and help relieve the economical burden that MDR organisms have on the global health care system.”
The article appeared on Medical Xpress.