A new study from researchers at the University of California, Davis, has found that monoclonal antibodies prevent lung and brain inflammation in aged, diabetic rhesus macaque monkeys with COVID-19 infection, according to Science Daily.
The study, published last month in the journal Cell Reports, has shown that neutralizing antibodies prevent the adverse inflammatory consequences of the coronavirus infection, according to the authors.
The findings explain how antibodies, whether naturally induced or vaccine-induced, or given as a treatment, can affect the course of the disease.
The researchers said the findings also suggest that antibodies could be given as a preventative treatment to high-risk people, such as older people who are in a nursing home.
Study investigator SmitaIyer said, “COVID-19 is more severe in elderly people and those with pre-existing conditions. The elderly and diabetics tend to be immunosuppressed, but if you can get antibody levels high enough, you can prevent severe infection.”
Vaccine-induced immune responses are very effective at preventing severe disease and death. However, an overwhelming inflammatory immune response could also be responsible for much of the damage of severe infections, according to Science Daily.
Iyer said, “We want to know, what are the immune determinants of disease.”
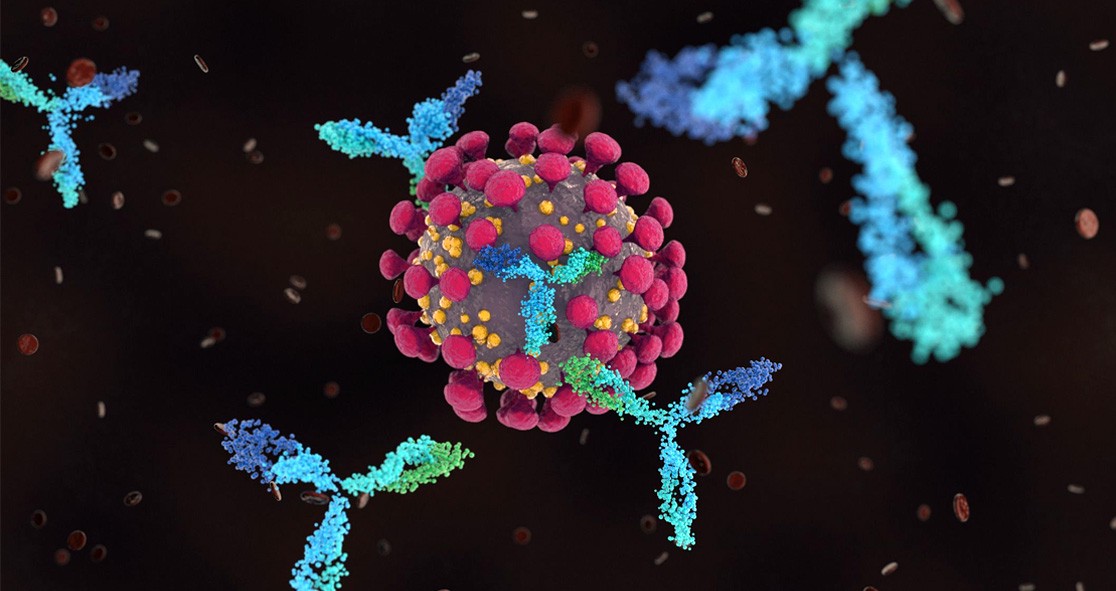
Iyer and colleagues studied two human monoclonal antibodies that target the spike protein of SARS-CoV-2 virus in aging, diabetic rhesus macaques. The animals were treated with antibodies three days before being infected with the coronavirus.
The COVID infections in rhesus macaques were generally mild, especially in those who were given monoclonal antibodies prior to the infection. The animals who were in the control group had more signs of lung inflammation.
The researchers found that animals who were not given monoclonal also had inflammation of the cerebrospinal fluid, while those treated with antibodies did not show inflammation in the cerebrospinal fluid.
These inflammatory conditions in the central nervous system might be connected to neurological symptoms of COVID-19 disease in humans, which explains why most people experience “long COVID” months after infection.